Pancreatic Clinics
Pancreatic Clinics
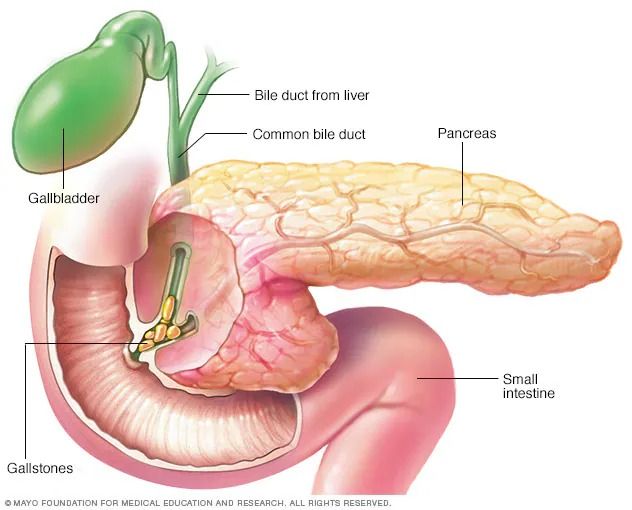
Pancreatitis is the inflammation of the pancreas, a gland located behind the stomach that plays a crucial role in digestion and blood sugar regulation. The condition can be acute, with a sudden onset and short duration, or chronic, developing over time and causing long-term damage.
Acute pancreatitis often occurs due to gallstones blocking the pancreatic duct or excessive alcohol consumption, though other causes include certain medications, infections, trauma, or high triglyceride levels. Symptoms typically include severe upper abdominal pain that may radiate to the back, nausea, vomiting, fever, and a swollen abdomen. Chronic pancreatitis, on the other hand, often results from prolonged alcohol use, genetic factors, or autoimmune diseases. It is marked by persistent pain, malabsorption of nutrients, and diabetes due to the progressive loss of pancreatic function.
Diagnosis involves blood tests to check elevated levels of pancreatic enzymes (amylase and lipase), imaging studies like CT scans, MRI, or ultrasound, and, in some cases, endoscopic procedures to assess the ducts.
Treatment depends on severity. Mild cases of acute pancreatitis may resolve with fasting, intravenous fluids, and pain management. Severe cases may require hospitalization, nutritional support, or surgery to address complications like infected pancreatic tissue or pseudocysts. Chronic pancreatitis management focuses on pain relief, enzyme replacement therapy to aid digestion, dietary adjustments, and treatment for diabetes if it develops.
Complications of pancreatitis include infections, organ failure, malnutrition, and an increased risk of pancreatic cancer. Preventative measures include avoiding excessive alcohol consumption, maintaining a healthy diet, managing gallstones, and controlling triglyceride levels.
Pancreatitis can significantly impact quality of life, particularly in chronic cases. Early diagnosis, appropriate treatment, and lifestyle changes are critical to managing the condition and preventing severe complications.
Pancreatic clinics specialize in diagnosing and treating diseases of the pancreas, including:
- Pancreatitis (acute and chronic)
- Pancreatic cysts
- Pancreatic cancer
- Neuroendocrine tumors of the pancreas
- Exocrine pancreatic insufficiency
- Complications related to pancreatic surgery.
Symptoms can vary depending on the specific condition, but common ones include:
- Severe abdominal pain (often radiating to the back)
- Nausea and vomiting
- Weight loss
- Jaundice (yellowing of the skin and eyes)
- Diabetes (new onset or worsening)
- Steatorrhea (oily, foul-smelling stools)
- Diagnosis typically involves:
- Blood tests (amylase, lipase, tumor markers)
- Imaging studies (CT scan, MRI, endoscopic ultrasound (EUS))
- Endoscopic retrograde cholangiopancreatography (ERCP)
- Biopsy (obtained through EUS or surgery)
Treatment varies depending on the condition and can include:
- Pain management
- Enzyme replacement therapy (for exocrine insufficiency)
- Medications to manage diabetes
- Endoscopic procedures (ERCP, EUS-guided interventions)
- Chemotherapy, radiation therapy, or surgery for pancreatic cancer.
- Surgical interventions for cysts, or chronic pancreatitis.
- You should see a pancreatic specialist if you experience:
- Persistent abdominal pain
- Unexplained weight loss
- Jaundice
- New-onset diabetes
- Any concerns about your pancreatic health.