Endoscopy
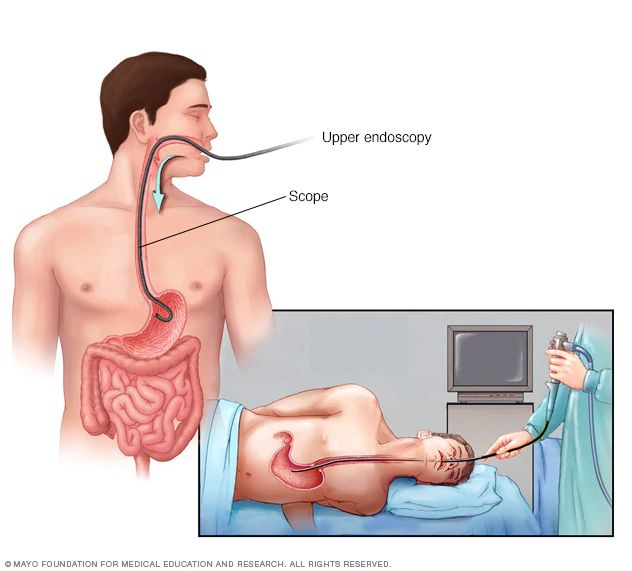
Endoscopy
The upper gastrointestinal (GI) endoscopy procedure is typically performed as an outpatient measure and necessitates minimal preparation apart from a fasting period prior to the procedure. Patients are ensured comfort through the administration of sedation or local anesthesia. Beyond diagnostics, upper GI endoscopy serves a therapeutic purpose. It allows doctors to conduct biopsies, extract foreign objects, widen narrowed sections, staunch bleeding, or eliminate abnormal growths like polyps.
This procedure is regarded as safe, with a low incidence of complications such as bleeding, infection, or perforation. The majority of patients recuperate swiftly and can resume their regular activities within a day.
Technological advancements in endoscopy, including high-definition imaging and narrow-band imaging, have significantly enhanced the precision and efficacy of the procedure. Upper GI endoscopy holds a pivotal position in modern medicine by affording a direct and intricate view of the upper digestive tract, aiding in early diagnosis, treatment, and disease prevention. Periodic endoscopic assessments are recommended for individuals with specific risk factors, ensuring enhanced long-term gastrointestinal health.
- Preparation varies depending on the type of endoscopy. Common steps include:
- Fasting.
- Bowel preparation (for colonoscopy/sigmoidoscopy).
- Adjusting medications.
- Following the doctors instructions.
Most endoscopies are not painful. Sedation or anesthesia is typically used to minimize discomfort.
The duration varies from 15 minutes to over an hour, depending on the procedure.
Risks are generally low but can include:
- Bleeding.
- Infection.
- Perforation.
- Adverse reaction to sedation.
- After the procedure:
- Recovery in a monitored area.
- Possible mild discomfort.
- Need for someone to drive you home.