Inflammatory Bowel Disease (IBD) Clinics
Inflammatory Bowel Disease (IBD) Clinics
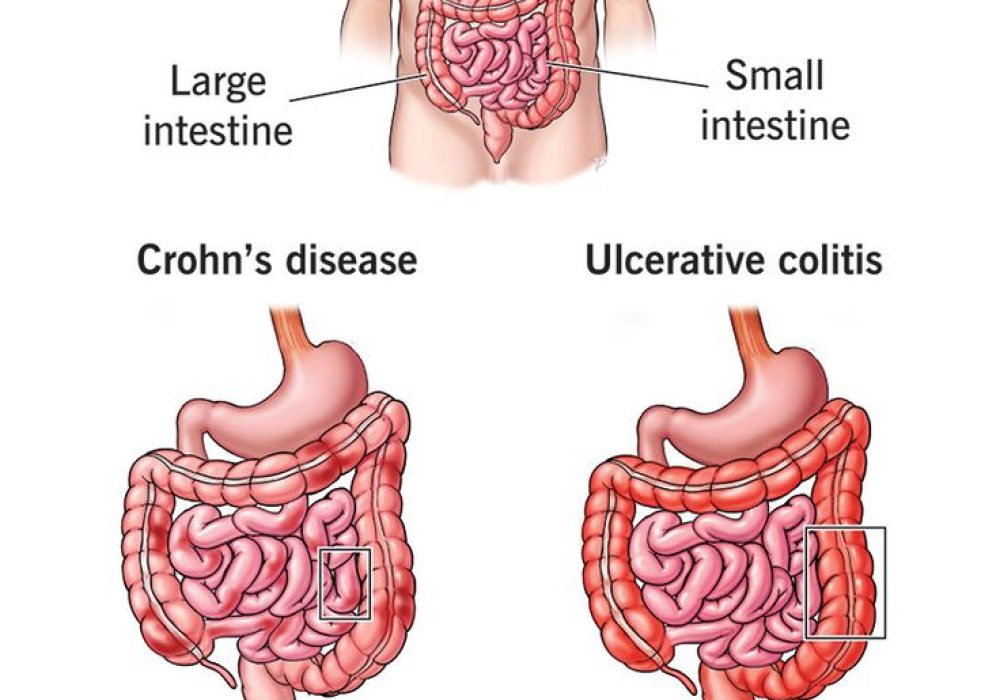
Inflammatory Bowel Disease (IBD) is a group of chronic inflammatory conditions that affect the gastrointestinal (GI) tract. The two main types are Crohn’s disease and ulcerative colitis. While Crohn’s disease can involve any part of the GI tract from the mouth to the anus, it most commonly affects the small intestine and colon. Ulcerative colitis, on the other hand, is limited to the colon and rectum and typically affects only the innermost lining of the bowel.
The exact cause of IBD is not fully understood, but it is believed to result from a combination of genetic predisposition, an abnormal immune system response, and environmental triggers. In IBD, the immune system mistakenly attacks the GI tract, leading to inflammation, damage, and symptoms such as abdominal pain, diarrhea (sometimes with blood), fatigue, weight loss, and reduced appetite.
Diagnosis involves a thorough evaluation, including blood tests, stool tests, endoscopy, colonoscopy, imaging studies (CT or MRI), and biopsies to assess the extent and nature of inflammation.
Treatment aims to reduce inflammation, manage symptoms, and prevent complications. It often includes anti-inflammatory drugs, immunosuppressants, or biologic therapies that target specific components of the immune system. In some cases, surgical intervention may be necessary to remove severely damaged sections of the bowel or treat complications like strictures, fistulas, or abscesses.
IBD can significantly impact a patient’s quality of life, with flares of active disease followed by periods of remission. Complications include malnutrition, anemia, intestinal blockages, and an increased risk of colorectal cancer.
While there is no cure for IBD, advances in treatment have improved outcomes, helping many patients achieve long-term remission. Lifestyle changes, dietary adjustments, stress management, and regular medical care are critical in managing this complex condition.
Inflammatory Bowel Disease (IBD) is a chronic inflammatory condition of the gastrointestinal tract. The two main types are Crohn's disease and ulcerative colitis. Unlike Irritable Bowel Syndrome (IBS), which is a functional disorder, IBD involves structural damage and inflammation of the bowel wall. IBS does not cause inflammation or ulcers.
Common symptoms include persistent diarrhea, abdominal pain, rectal bleeding, weight loss, fatigue, and urgency to have a bowel movement. Symptoms can vary depending on the severity and location of the inflammation. Crohn's disease can affect any part of the GI tract, while ulcerative colitis is limited to the colon and rectum.
Diagnosis typically involves a combination of medical history, physical examination, blood tests, stool tests, and imaging studies such as colonoscopy or sigmoidoscopy with biopsies. Sometimes, imaging like CT or MRI enterography may be required.
Treatment aims to reduce inflammation, manage symptoms, and prevent complications. Options include:
- Medications: Aminosalicylates, corticosteroids, immunomodulators (like azathioprine or methotrexate), and biologics (like TNF inhibitors, integrin blockers, and IL-12/23 inhibitors).
- Dietary modifications: Tailored diets to manage symptoms and ensure adequate nutrition.
- Surgery: In severe cases, surgery may be necessary to remove damaged portions of the intestine.
- Therapeutic endoscopy: Stricture dilation, and other endoscopic interventions.
If you experience persistent abdominal pain, changes in bowel habits, rectal bleeding, or unexplained weight loss, it's essential to seek medical attention from a gastroenterologist.
Many medications used to treat IBD are safe for long-term use. However, they can have potential side effects, so regular monitoring by a gastroenterologist is important. The benefits of controlling the disease usually out weigh the risks of the medication.