Liver Transplantation
Liver Transplantation
Liver transplantation is a life-saving surgical procedure in which a diseased or failing liver is replaced with a healthy liver from a donor. It is typically performed for patients with end-stage liver disease, acute liver failure, or certain types of liver cancer. Common causes leading to the need for a transplant include cirrhosis from chronic hepatitis (e.g., hepatitis B or C), alcoholic liver disease, non-alcoholic fatty liver disease (NAFLD), autoimmune liver diseases, and genetic conditions like Wilson’s disease.
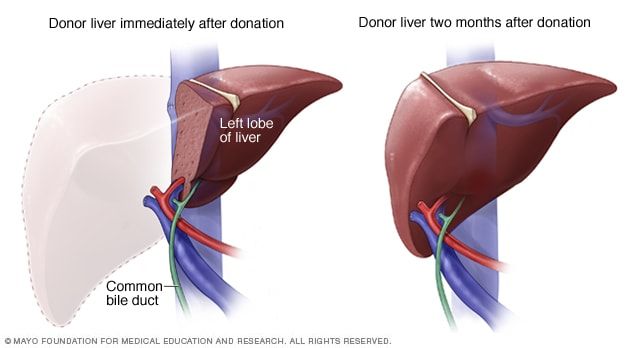
Liver transplants use either a deceased donor liver or a portion of a liver from a living donor. Since the liver can regenerate, living donor transplants involve removing part of the donor’s liver, which grows back to normal size in both the donor and recipient over time. The surgical procedure is complex, requiring skilled teams to remove the damaged liver and attach the donor liver to the recipient’s blood vessels and bile ducts.
Recipients must undergo thorough medical evaluations to ensure they are suitable candidates for transplantation. Post-transplant, patients take immunosuppressive medications to prevent organ rejection, along with regular monitoring to manage complications and ensure proper liver function.
Although liver transplantation is highly effective, risks include rejection, infections, bleeding, or bile duct complications. Advances in surgical techniques, donor matching, and immunosuppressive therapies have significantly improved success rates, with many patients experiencing long-term survival and restored quality of life.
Liver transplantation is a critical option for individuals with irreversible liver damage. However, organ shortages remain a significant challenge, emphasizing the importance of organ donation awareness. For patients and their families, liver transplantation offers hope and a chance for a healthier, extended life, underscoring its pivotal role in modern medicine.
- Common conditions that may necessitate a liver transplant include:
- Cirrhosis (from various causes like hepatitis C, alcoholic liver disease, NAFLD/NASH)
- Acute liver failure
- Hepatocellular carcinoma (liver cancer)
- Autoimmune liver diseases (primary biliary cholangitis, primary sclerosing cholangitis, autoimmune hepatitis)
- Genetic liver diseases (Wilson's disease, hemochromatosis)
- Cirrhosis (from various causes like hepatitis C, alcoholic liver disease, NAFLD/NASH)
The evaluation process is thorough and includes:
- Medical history and physical examination.
- Blood tests (liver function, blood type, viral screening).
- Imaging studies (ultrasound, CT scan, MRI).
- Cardiac and pulmonary function tests.
- Psychosocial evaluation.
- Listing on the transplant waiting list.
There are two main types:
- Deceased donor: A liver from a person who has died and donated their organs.
- Living donor: A portion of the liver is removed from a healthy living person and transplanted into the recipient.
- The diseased liver is removed, and the donor liver is placed in the recipient's abdomen. The blood vessels and bile ducts are connected.
- Risks include:
- Rejection of the transplanted liver.
- Infection.
- Bleeding.
- Bile duct complications.
- Side effects from immunosuppressant medications.